Introduction In the dynamic and margin-pressured world of modern healthcare, Artificial Intelligence (AI) is no longer a fringe experiment—it is a critical investment. However, for every CEO and COO managing a healthcare organization, the imperative remains the same: demonstrate a clear, quantifiable Return on Investment (ROI). Automating operations with AI for the sake of automation […]

Introduction
In the dynamic and margin-pressured world of modern healthcare, Artificial Intelligence (AI) is no longer a fringe experiment—it is a critical investment. However, for every CEO and COO managing a healthcare organization, the imperative remains the same: demonstrate a clear, quantifiable Return on Investment (ROI).
Automating operations with AI for the sake of automation is a strategy doomed from that start. The true value lies not in the technology itself, but in a rigorous, executive-level framework that links AI Operations (AI Ops) directly to reduced administrative spend, improved patient outcomes, and mitigated compliance risk.
This is the strategic mandate: Quantify Before You Automate.
The Strategic Challenge: AI Hype vs. Healthcare Reality
The market confirms the urgency: the global AI in healthcare market is projected to reach over $500 billion by 2032 (Fortune Business Insights, cited by NASDAQ). Yet, for executives, where operating costs and regulatory pressure are highest, AI Ops must move beyond simple task automation to addressing systemic, high-value problems such as:
- Prior Authorization Backlogs: Directly impacting physician satisfaction and cash flow.
- Predictive Revenue Cycle Management (RCM): Forecasting claim denials and improving collections.
- Compliance and Risk Monitoring: Real-time auditing for Third-Party Administrators (TPAs) and health plans to flag regulatory violations before they incur penalties.
For many organizations, the promise of AI remains stalled at the Proof-of-Concept (PoC) stage. Gartner advises that traditional ROI models often overlook the non-financial returns of AI, emphasizing the need to adapt evaluation frameworks to account for strategic, operational, and risk-reduction impacts.
As Forbes highlights, the greatest barrier to realizing AI value is not the technology, but the failure to integrate it thoughtfully into complex existing workflows and establish proper measurement from the outset. In other words, AI is no different than any traditional software project that starts at the need and has a hypothesis for changes that result in cost reduction, value creation or compliance.
The Serious Development ROI Framework: Three Pillars of Quantificationtage
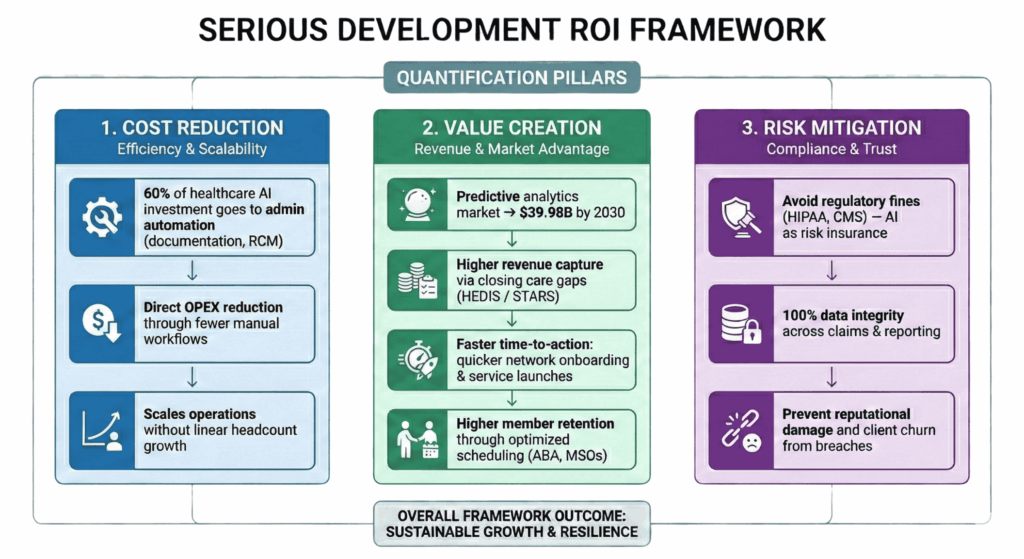
A successful Healthcare AI Ops initiative is built on a foundation of measurable business metrics, not technical specifications. We propose a three-pillar framework for establishing and measuring ROI before the first line of code is deployed.
1. The Cost-Reduction Pillar (Efficiency & Scalability)
Focus on the tangible financial savings. AI investments in administrative tasks like documentation and RCM have attracted 60% of all healthcare AI investment (Vention), underscoring the priority C-suites place on operational efficiency.
| Key Metric | Definition & Impact | Example for MSO |
|---|---|---|
Cost-Per-Transaction Reduction | Decrease in the fully loaded cost of a single process (e.g., handling a prior authorization request). | Reducing the cost to process a complex claim from $15.00 to $3.50 through document ingestion AI. |
| FTE (Full-Time Equivalent) Avoidance/Redeployment | Calculating the headcount costs saved or moved to higher-value roles (e.g., patient engagement). | Avoiding the hire of 10 new RCM analysts by deploying AI for denial prediction and automated appeals. |
| Error Rate Reduction | Decrease in errors leading to costly reprocessing, fines, or patient dissatisfaction. | Reducing the claim denial rate by 5% due to AI-driven completeness checks. |
2. The Value-Creation Pillar (Revenue & Market Position)
This pillar focuses on how AI creates new revenue or competitive advantage. The Predictive Analytics in Healthcare Market, driven by AI, is projected to nearly triple to $39.98 Billion by 2030 (GlobeNewswire)—evidence that forecasting and proactive care are driving market value.
- Increased Revenue Capture: Using AI to identify and close care gaps in quality programs (like HEDIS/STARS), directly increasing bonus payments for health plans.
- Faster Time-to-Action: Cutting the time required to onboard a new provider network or roll out a new service offering, giving a competitive edge.
- Customer/Member Loyalty: For Applied Behavior Analysis (ABA) providers, using AI Ops to optimize therapist scheduling and reduce administrative friction, leading to higher retention rates and better outcomes.
3. The Risk-Mitigation Pillar (Compliance & Security)
Quantifying risk reduction is essential, especially for organizations managing sensitive Dual-eligible plans.
- Compliance Fine Avoidance: Calculating the expected loss from potential regulatory fines (e.g., HIPAA violations or CMS non-compliance) and the cost of the AI solution as an insurance premium against that loss.
- Reputational Risk Reduction: For TPAs, using AI to ensure 100% data integrity and regulatory adherence, avoiding the negative media and client churn associated with a security or compliance breach.
Case in Point: The Serious Development Impact
At Serious Development, we've repeatedly seen this ROI-first approach turn abstract AI investments into concrete balance sheet improvements.
For example, a prominent East Coast healthcare organization came to us struggling with operational bottlenecks that hampered their ability to scale. By applying a tailored AI Ops strategy, we focused not just on process automation, but on the three-pillar ROI framework outlined above. The result was a dramatic improvement in efficiency, allowing them to redeploy talent to patient care initiatives.
"We moved beyond 'proof-of-concept' to a quantifiable 'proof-of-value' strategy, ensuring every dollar spent on AI delivered a measurable return against operational expenditure."
— Serious Development Case Study (See our full case study on a similar healthcare digital transformation project here).
Your Next Strategic Move: Start with the Metrics, Not the Code
The shift to true Healthcare AI Ops requires leadership to commit to a metrics-driven culture. This means dedicating resources to data quality and process mapping before purchasing software.
To move your organization from aspiration to execution, start by auditing your current operational friction points and quantifying their exact financial impact. Over 80% of healthcare executives who track AI outcomes report a moderate or high ROI, with many seeing returns in under 12 months (Vention). The time to strategize is now.
Don't automate blindly. Quantify strategically.
Frequently Asked Questions (FAQ)
My CIO/CTO says we need AI Ops. What does ROI actually look like for healthcare process automation?
The ROI for Healthcare AI Ops isn't just about saving money (cost-reduction); it's about creating new value and mitigating regulatory risk. Quantifiable ROI looks like a 10% reduction in denied claims, a 25% decrease in cost-per-transaction, or achieving 100% real-time compliance auditing—which prevents multi-million dollar fines. If the business case focuses solely on FTE reduction, the initiative is likely too narrow.
What is the single biggest risk to AI adoption in Medicare Advantage/Health Plans?
The single biggest risk is poor quantification and data governance upfront. Without a rigorous framework to define and measure success (like the three-pillar model), AI projects get stuck in 'pilot purgatory.' Gartner highlights that the failure to restructure existing processes around the AI is a common pitfall. For Medicare Advantage plans, specifically, the risk is failing to align AI with STARS Rating improvement (Value Creation Pillar), thereby leaving significant revenue on the table.
I'm a COO at an MSO. How do I convince my board to fund a complex AI Ops project?
You secure funding by translating the technology into a language the board understands: financial impact and minimized liability. Frame the investment not as an IT spend, but as a Compliance and Scalability Insurance Policy. Use the Cost-Reduction and Risk-Mitigation Pillars to build your case. Specifically, calculate the opportunity cost of not automating (e.g., projected penalty fines + lost revenue from manual claim processing) and present the AI spend as a smaller, predictable alternative.
What is an 'AI Ops Framework' and why is it essential before buying automation software?
An AI Ops framework (like our Three-Pillar Model) is a strategic blueprint that defines what success looks like before you integrate technology. It's essential because it forces your organization to:
Align AI deployment with measurable executive goals (e.g., reducing operational leverage). Without this framework, you risk solving the wrong problem or implementing a solution that can't be objectively judged as successful.
Identify the highest-value friction points (e.g., $5M in denied claims vs. $50k in manual email sorting).
Establish baseline metrics (Quantify Before You Automate).
Sources
- Fortune Business Insights / NASDAQ. (2025). Global AI in Healthcare Market Projection. [Citation for market reaching over $500B by 2032].
- Gartner. (2024). Optimize AI Investments for Long-Term Business Growth. [Citation supporting the need to adapt ROI frameworks for strategic, non-financial returns].
- Forbes. (2024/2025). Implementing AI In Healthcare Requires Overcoming These Five Challenges. [Citation supporting the challenge of integrating AI into complex workflows].
- Vention. (2025). AI in Healthcare Statistics: Market Size, Adoption, Impact. [Citation for 60% of investment flowing to administrative AI and 80% reporting ROI].
- GlobeNewswire. (2025). Predictive Analytics in Healthcare Analysis Report 2025. [Citation for the market projected to reach $39.98 Billion by 2030].






